Fibrosis Explained: Objective Post-Surgical Scar Assessment Using the SkinFibroMeter™
- Emma Danciu
- Dec 31, 2025
- 6 min read
Updated: Jan 2
Understanding Fibrosis — with Context for SkinFibroMeter Assessment
Fibrosis is the excessive accumulation of fibrous connective tissue—mainly collagen—formed as the body attempts to repair an injury. It’s essentially wound healing gone into overdrive.
Instead of restoring normal tissue architecture, the body deposits too much collagen, creating stiff, dense tissue that can interfere with normal function.
You can think of it as scar tissue that didn’t know when to stop growing.
Fibrosis is the end result of a persistent or exaggerated inflammatory response. When tissue is injured, the body calls in fibroblasts to rebuild the area. Normally these fibroblasts produce collagen and then stop.
But if inflammation is prolonged—or the healing environment is disrupted—fibroblasts keep producing collagen, turning a temporary matrix into permanent scar-type tissue.
Common triggers include:
Chronic inflammation
Repeated injury
Infection
Radiation therapy
Metabolic disorders
Surgery (a major driver)
Fibrosis in Post-Surgical Scarring
After surgery, fibrosis is part of normal scar formation. But it becomes clinically relevant when the process becomes excessive, disorganized, or prolonged.
How It Develops:
Tissue is cut/disrupted → immediate inflammation
Fibroblasts flood the area → collagen deposition
Angiogenesis occurs → early scar is vascular and soft
Remodeling phase (months to years) → collagen becomes denser and more aligned
If the healing process becomes overly aggressive or poorly regulated, the scar can progress into fibrosis—a state where the tissue becomes abnormally dense and rigid.
This often results in thick, firm, or cord-like areas that alter the normal architecture of the skin and underlying structures. As fibrosis develops, patients may experience restricted movement and reduced tissue pliability, making the affected area feel tight or unyielding.
The excessive collagen deposition can also cause pain or nerve tethering, as scar tissue adheres to deeper layers.
In more advanced cases, fibrosis may contribute to edema or lymphatic impairment, which is particularly important to recognize in the context of lymphedema assessment and management. Read more about lymphedema assessment and management with the LymphScanner. |
Fibrosis tends to appear more commonly after certain types of surgical procedures. It is frequently observed following post-mastectomy or other breast surgeries, particularly in the axilla and chest wall, as well as after abdominal procedures such as C-sections, or hernia repairs.
It can also develop after liposuction or body contouring procedures and orthopedic surgeries, including operations on the knee or shoulder.
Additionally, any surgery that involves drains, seromas, or wound complications increases the risk of excessive fibrotic tissue formation, as these factors can prolong inflammation and disrupt normal healing.
Why does fibrosis matters clinically
Post-surgical fibrosis is clinically important because it can impair lymphatic flow, contribute to swelling, reduce tissue mobility, cause discomfort, and limit function, while also affecting aesthetic outcomes and potentially complicating future interventions.
Quantify Fibrosis, Track Progress and Optimize Care with the SkinFibroMeter™ |
The SkinFibroMeter™ provides objective, reproducible measurements of tissue stiffness, enabling clinicians to:
Detect early fibrosis before complications arise
Map distribution of fibrotic tissue
Track treatment efficacy (manual therapy, lymphatic drainage, physiotherapy, laser, or aesthetic interventions)
Standardize assessments across visits and clinicians
The SkinFibroMeter™ is a compact, wireless, non-invasive device designed to quantify skin and subcutaneous tissue stiffness, which correlates with fibrotic changes. It converts mechanical resistance of the tissue into measurable numerical data.
With its indentation-based technology, it allows clinicians to objectively assess tissue stiffness and areas of induration, providing a reliable measure of fibrosis.
By using this Instrument, they can detect early signs of abnormal scar formation, monitor progress during anti-fibrotic therapies, such as manual therapy or lymphatic drainage. They can also identify localized dense areas that may correspond to adhesions or edema, enabling more precise treatment planning and follow-up.
Let’s take a closer look at how the device works and what makes it scientifically reliable
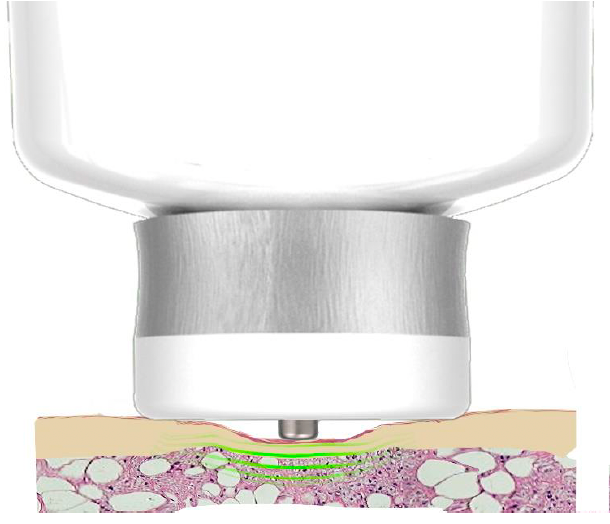
Measurement Principle
The probe is pressed quickly against the skin surface and the speed is precisely controlled by the Instrument to apply consistent force.
The specially-designed indenter senses the force against the indurated tissue when the pressure-controlled base plate is in full contact with the skin.

As the probe measures into the tissue, the SkinFibroMeter™ assesses how much the skin deforms under the load.
Calculation of Tissue Stiffness
The force against an indurated area is determined from the characteristics of the total force-to-indenter force curve at the moment a full contact between the base plate and skin is reached.
The skin and the underlying upper subcutis resist the deformation and the induration value in Newtons (N) is determined.

Total force = indenter force + base plate force
The SkinFibroMeter™ doesn’t just measure the force and displacement—it also interprets the data using advanced computer simulations. Specifically, Finite Element (FE) analysis, a method engineers use to simulate how complex structures deform under stress, is applied here to model the skin and underlying tissue as a 3D structure.
Essentially, it creates a virtual 3D model of skin’s response to the force, allowing precise calculation of properties like stiffness, elasticity, or fibrosis.
The SkinFibroMeter™ measures force(N) against
indurated subcutis(at depth> 2 mm)
Practical Applications for Clinicians
Aesthetic Clinicians:
Track post-procedure scar healing (liposuction, abdominoplasty, breast aesthetics)
Optimize manual therapy, microneedling, or laser treatments
Oncology Rehab Specialists:
Monitor post-mastectomy fibrosis and lymphatic flow
Identify early lymphedema risk
Physiotherapists:
Assess joint mobility limitations caused by fibrotic tissue
Track rehabilitation progress objectively
Reconstructive & Plastic Surgeons:
Evaluate transplanted tissue healing
Objectively measure post-reconstruction scar stiffness to support accurate post-surgical skin assessment.
Plan secondary interventions (scar revision, laser therapy, physiotherapy)
Optimize functional and aesthetic outcomes
Key Takeaways: Why the SkinFibroMeter Stands Out
Fibrosis represents a maladaptive form of wound healing characterized by excessive collagen deposition, increased tissue stiffness, and altered biomechanical properties that can impair function, aesthetics, and long-term recovery.
Because these structural changes often progress gradually and may not be apparent through visual inspection or palpation alone, objective quantification is essential for early detection and effective intervention.
The SkinFibroMeter™, through its standardized indentation technology, provides a reliable, reproducible measure of tissue stiffness and induration, offering clinicians a precise method to assess the presence and severity of fibrosis.
By converting mechanical resistance into quantifiable data, it enables clinicians to identify abnormal scar development earlier, monitor changes over time, and evaluate the effectiveness of therapeutic strategies such as manual therapy, lymphatic techniques, laser treatments, or postoperative rehabilitation.
Incorporating objective stiffness measurement into routine clinical practice with the SkinFibroMeter™ enhances decision-making, supports more personalized treatment plans, and improves communication between multidisciplinary teams.
Ultimately, the use of the SkinFibroMeter™ as part of fibrosis assessment helps clinicians achieve better functional, aesthetic, and long-term outcomes for patients, making it a valuable and increasingly necessary tool in modern postoperative and scar-management care.
Elevate your clinical practice
Trust the SkinFibroMeter™ for precise, scientific fibrosis assessment.
Discover Delfin’s full range of skin research Instruments at Skinlabs and see how advanced measurement tools can elevate your next research. |
PUBLICATIONS
PUBMED
Seo SR, Kang NO, Yoon MS, Lee HJ, Kim DH. Measurements of scar properties by SkinFibroMeter®, SkinGlossMeter®, and Mexameter® and comparison with Vancouver Scar Scale. Skin Res Technol. 2017 Aug;23(3) :295-302. doi: 10.1111/srt.12334. Epub 2016 Oct 30. PMID: 27796064.
PUBMED
Sun D, Yu Z, Chen J, Wang L, Han L, Liu N. The Value of Using a SkinFibroMeter for Diagnosis and Assessment of Secondary Lymphedema and Associated Fibrosis of Lower Limb Skin. Lymphat Res Biol. 2017 Mar;15(1):70-76. doi: 10.1089/lrb.2016.0029. Epub 2017 Mar 9. PMID: 28277926.
TAYLOR & FRANCIS
Ohkubo, J. ichi, Wakasugi, T., Takeuchi, S., Takahashi, A., Nguyen, T. N., & Suzuki, H. (2022). Biophysical properties of the neck skin indicating potential complications of salvage surgery for laryngeal/hypopharyngeal cancer. Acta Oto-Laryngologica, 142(7–8), 634–637.
JOURNAL OF BIOPHOTONICS
Kurtti A, Nguyen JK, Weedon J, er al. Light emitting diode-red light for reduction of post-surgical scarring: Results from a dose-ranging, split-face, randomized controlled trial. J. Biophotonics. 2021; 14: e202100073.
AESTHETIC SURGERY JOURNAL
Mary E Ziedler, Brannon Claytor, Michaela Bell, Laurie Casas, Alan D Widgerow. Gene Expression Changes in the skin of Patients Undergoing Medial Thigh Liposuction With Pre-Surgical and Post-Surgical Application of Topical Products. Aesthetic Surgery Journal Open Forum, Volume 2, Issue 3, September 2020, ojaa033.




















Comments